Introduction
As is part of many engineering undergraduate degrees, the final year is spent doing a senior design project where the skills and knowledge we have gained over the prior few years will be applied to tackle an engineering problem. Personally, after working on multiple medical device projects, I looked forward to doing it now within the mentorship and guide of the academic curriculum. Seeing an opportunity to create a real and meaningful project, I asked fellow biomedical engineering students whether they would want to work together on a project that we would purposefully seek out with the University of Michigan Health System. We approached the course director and said we wanted to assemble our team months in advance of the academic year to begin working on a project together. From the get go, when we assembled our team, we made team chemistry a really important part of our mission, doing activities together, eating together, even exercising together (interestingly, it was through this experience that I was introduced to CrossFit through fellow classmate Julie Foucher).
With that, we identified an engineering mentor in Dr. James Ashton-Miller and a clinical mentor Dr. William Chey to tackle the problem of diagnosing dyssynergic defecation at the point-of-care with a low cost finger-based device (i.e. digital manometry) that could be used routinely by GI physicians.
Motivation
- Each year, 63 million Americans are affected by chronic constipation, and less than half of this constipation population seeks medical treatment.
- Of this treatment population, roughly half will improve with conventional dietary/laxative therapies while the other half of this population will not.
- The reason why this particular group does not improve with dietary/laxative therapies is because they suffer from a specific type of constipation known as dyssynergic defecation (DD).
Problem
- DD arises from muscle coordination issues in the anorectum, meaning problems with anal sphincter relaxation, puborectalis muscle relaxation, and/or intrarectal pressure generation during defecation.
- While DD cannot be treated with dietary/laxative therapies, studies have shown that biofeedback therapy—a type of physical training regimen—has an 80% positive response rate in DD patients.
- The current gold standard tool for diagnosing DD is anorectal manometry but its drawbacks include:
- high start-up and maintenance costs often exceeding $75,000 and $300,000 respectively complicated data analysis
- inability to assess puborectalis muscle activity and intrarectal pressure
- As a result of the high costs and expertise required to operate ARM, fewer than 200 clinics across the United States house ARM technology

Design
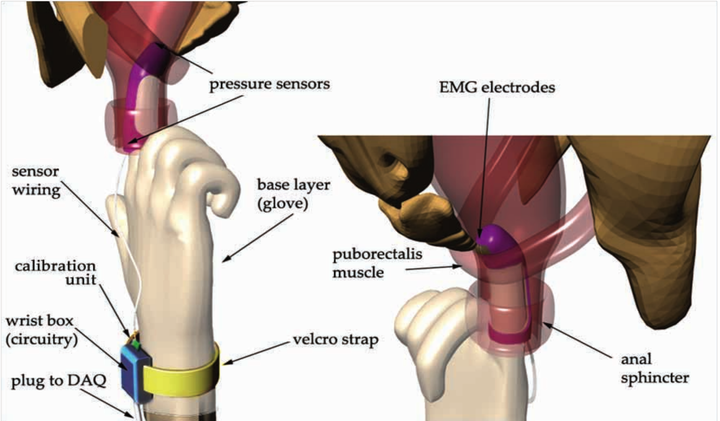
The essence of our solution was to create a wearable finger-based device to perform “digital manometry” that a GI physician could use to measure the coordination of the muscles of defecation. The finger portion of the device will be capable of simultaneously obtaining EMG biopotentials from the puborectalis muscle, fluid pressure in the intrarectal region, and contact pressure in the anal sphincter region.



This device would then interface through a Data Acquisition (DAQ) card to software that would determine whether these incoming signals were dis-coordinated as in the case of dysynnergic defecation.

To read more about our device, see the attached poster and presentation (at the top of this page).
At the end of the semester, we presented our results, and raised a Michigan Business Dare to Dream Grant after writing a business proposal around how to commercialize this device. After we graduated, Dr. William Chey and Dr. James Ashton-Miller continued to develop the idea within their labs. To date, this digital manometry device has an issued patent from the USPTO and a recent publication demonstrating similar evaluation of anorectal pressures and puborectalis myeloelectric activity at an order of magnitude less cost than high-resolution anorectal manometry.



