Magnetic Ventures

Intro to Engineering
It all began during an introduction to engineering course I was taking as a freshman in college at the University of Michigan. The course was meant to be a first glance at the design process to take a problem in the medical device space, apply principles of design engineering, and ultimately, propose a solution to a current problem our team had identified. Our team decided to tackle the problem of wear in artificial joints.
Background
Over the past century, total joint replacement has improved dramatically, from a risky experimental procedure to a commonplace surgery with initial success rates of over 90% (SCOI 2008). Artificial joints give arthritis-sufferers, trauma victims, and other patients a new lease on life and a restored degree of independence. In 2008, 1.3 million first-time (primary) total joint replacements were done in the United States (Frost & Sullivan 2007). Artificial knees and hips are the most mature devices in this field, and most have a plastic-on-metal interface. In 2008, 307,000 primary artificial hips and 608,000 primary artificial knees were implanted. Unfortunately, most plastic-on-metal joints are only temporary solutions. Many implants last only 10-15 years before a second surgery (revision surgery) is needed to replace the worn device. In 2008, 60,100 hip revisions and 43,600 knee revisions were done in the U.S. (Frost & Sullivan 2007). Approximately half of all knee revisions can be attributed to wear in the plastic part of the joint interface (Orozco 2002). High wear is also a leading cause of hip revisions (Cluett 2005). For the patient, a revision surgery means a longer hospital stay and another grueling recovery period. Revision surgery is also financially painful. The American Academy of Orthopedic Surgeons estimates that knee and hip revisions cost Medicare and private insurance companies about $3 billion each year (AAOS 2008).
Solution
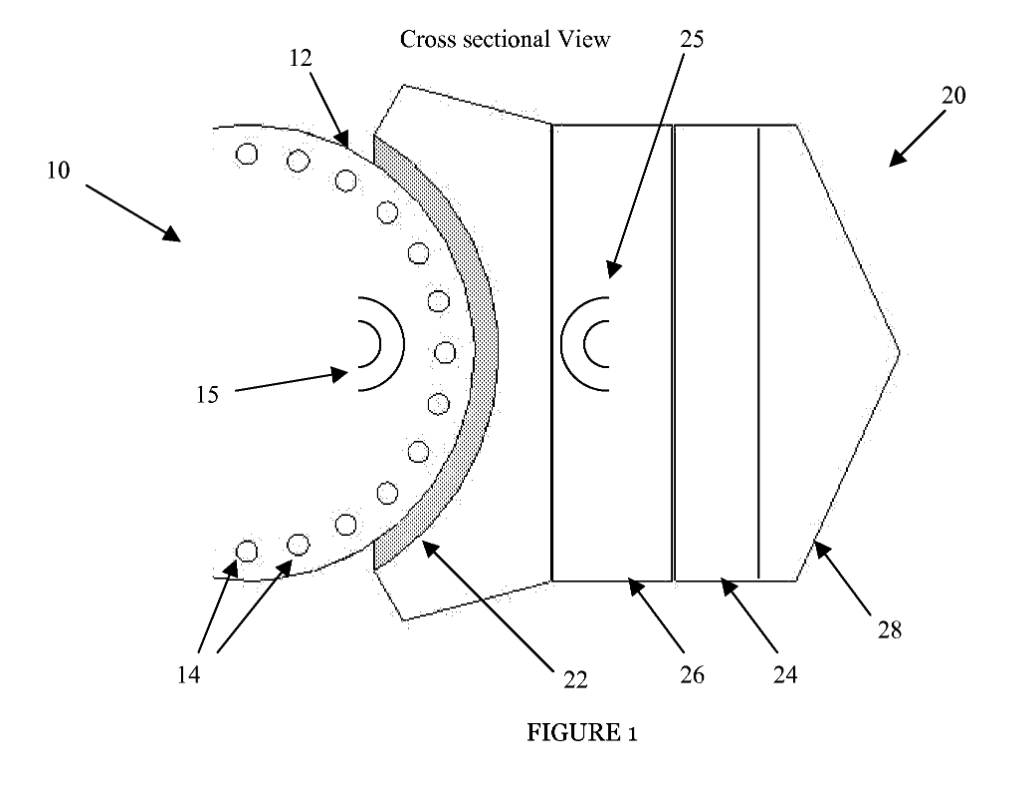
In order to solve this problem, I designed the Magnetically-Assisted Artificial Joint - a patent-pending improvement on plastic-on-metal knee and hip joints. This technology lowers the contact stress at the joint interface through the use of rare-earth neodymium magnets. It operates on a similar conceptual basis as MagLev, which utilizes electromagnetic forces to lower friction between the train and the track, thereby increasing efficiency. A MagLev track experiences constant load from the train, and the magnetic field needed to lift the train is constant. However, the artificial joint experiences dynamic loading; therefore, the system was designed to self-regulate the magnetic forces within the joint. The technology uses an elastic material as a regulatory material to control the distance between the magnets in the joint and adjust the magnetic force. As the force in the joint increases, the magnets are pushed closer together, lowering the interface force (normal force) and consequently decreasing the friction in the joint (as can be seen below).
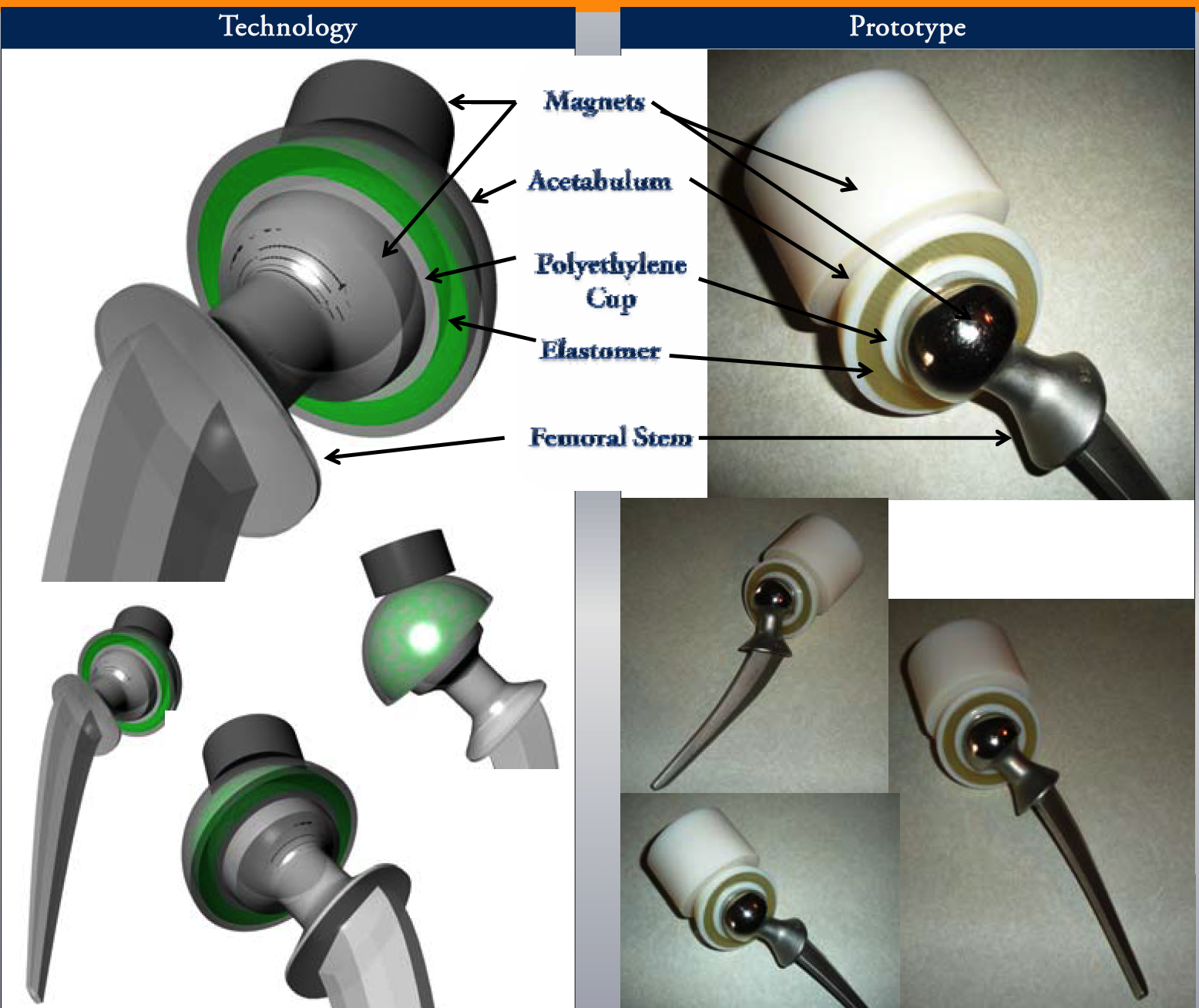
While our team of undergraduate students consisting of engineers and business students learned a lot through this process of trying to move an idea from concept to reality, and in so doing, won numerous business plan competitions (Michigan Business Challenge, 1000 pitches) along with multiple grants to fund development of the project (NCIIA E-Team Grant, Michigan Business School Dare to Dream Grant), the project ultimately proved to have significant hurdles in making it clinically feasible. Ultimately, this experience began my passion to tackle difficult problems but also taught me the value of clinical understanding in identifying the right problems and appropriate solutions.
Transition
In concluding the magnetically-assisted artificial joint, the orthopedic surgeon we were working with suggested using this technology we had developed within the construct of knee braces. He proposed that many individuals who wore them found them uncomfortable as the braces unloaded the knee joint in a static rather than dynamic manner (as our technology could potentially do).
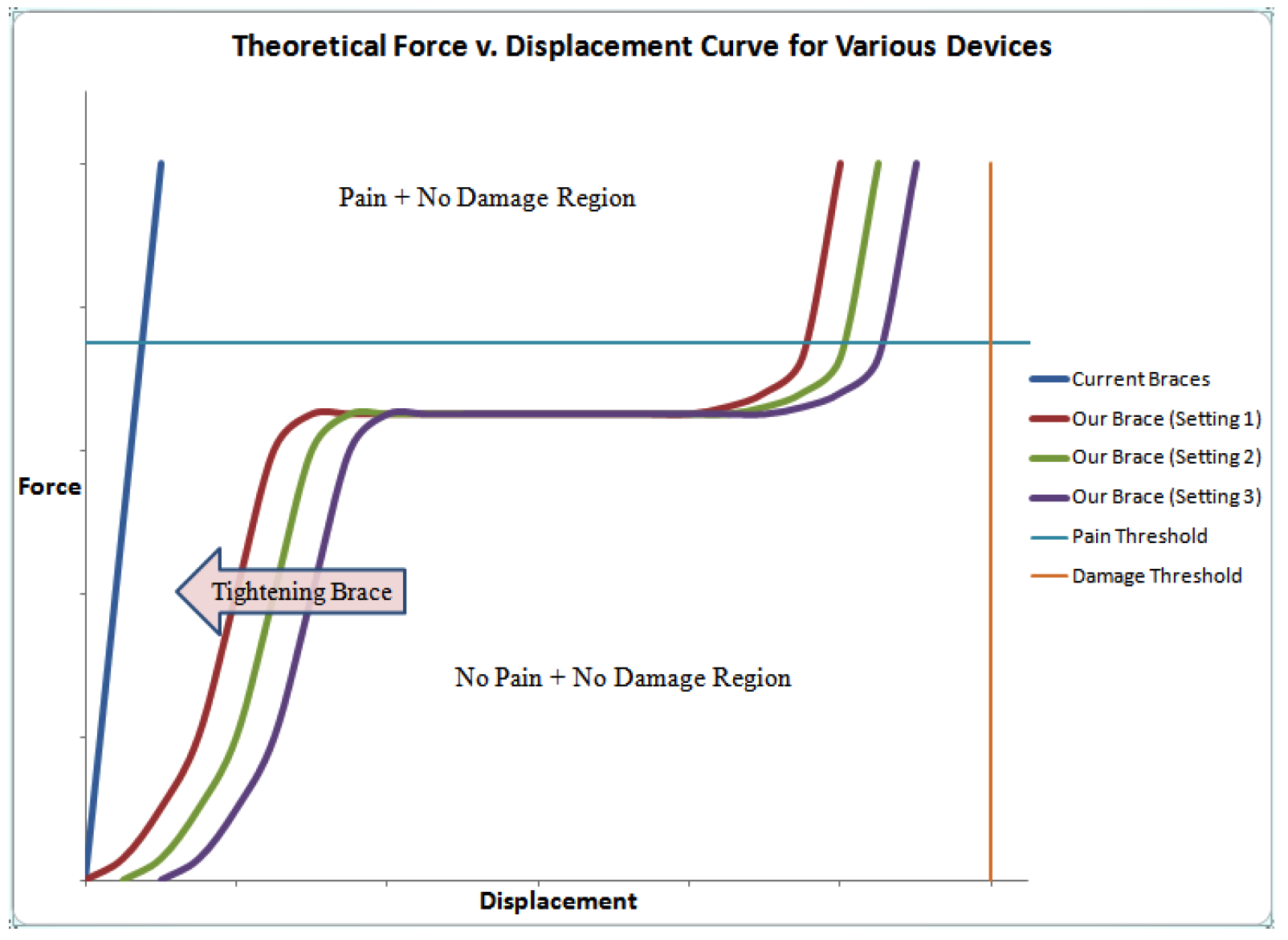
Current medial unloading OA knee braces provide a single, highly asymptotic unloading profile. A small displacement is met with a large force, resulting in rigid support. This profile is always identical, regardless of whether the patient is laying down, sitting, or standing. When the patient is participating in an activity which would see a high displacement, such as running, they are met with a large lateral force on the joint. This rigid reaction results in a painful scenario, leaving the patient with high levels of discomfort. This makes the patient unlikely to wear the brace during these high displacement activities, when they need the support the most.
Our technology (see full poster here) regulates the lateral force applied on the knee to keep the level of support comfortable and below the pain threshold throughout a wide range of activities. The system which regulates the lateral force consists of a Belleville washer in series with a magnet-elastomer-magnet subsystem (see below).
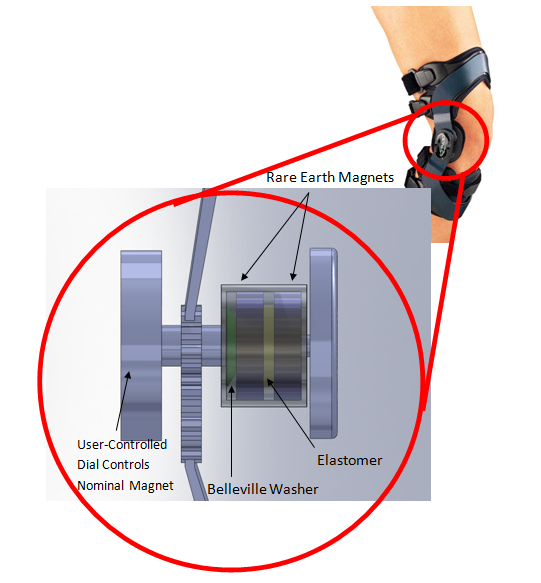
The resulting force unloading profile can be seen below. At a small displacement, the unloading profile is dominated by the magnet-elastomer-magnet combination. The effect of the system at a small displacement is a resultant load which ramps up gently, providing sufficient force to be supportive without being painful. At a moderate displacement, the effect of the Belleville washer begins to dominate, creating a plateau in the force-displacement curve. At this segment of the unloading profile, the Belleville washer is collapsing, resulting in a constant force at an increasing displacement. The washer is calibrated such that this plateau occurs just below the pain threshold. The system is continuing to support the knee without applying a painful lateral force. After the Belleville washer has fully collapsed, the force-displacement profile is once again dominated by the magnet-elastomer-magnet subsystem. The supportive force again begins to ramp up in relation to the displacement to ensure that the displacement in the knee does not reach a point where it is damaging to the joint.
In order to demonstrate the novelty of our technology, preliminary piston prototypes were built and their force profiles were characterized with an Instron device.
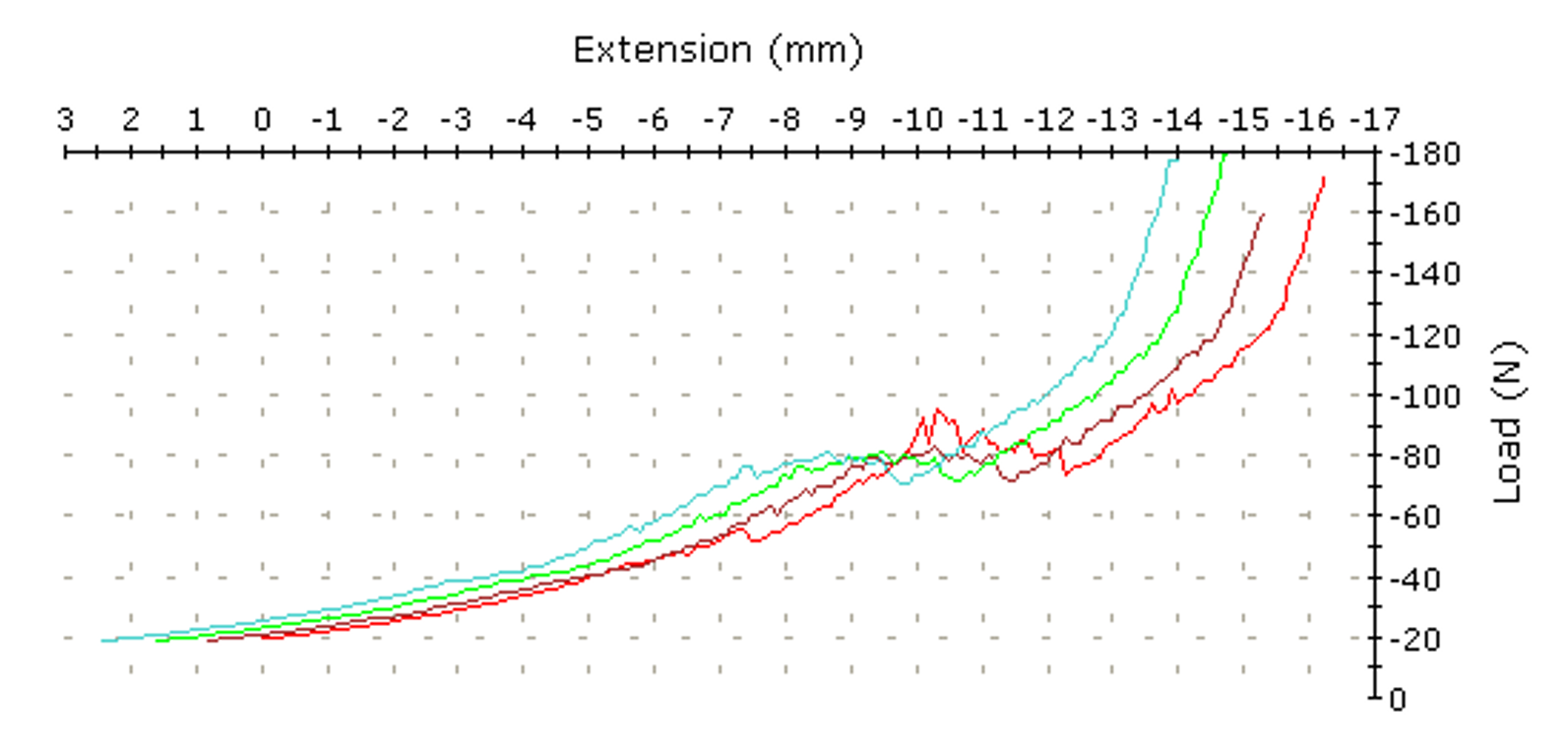
As we can see, when 3 belleville washers are assembled in series with two repulsive magnets within a cylinder piston encasing, we are able to generate cushioning force, followed by a force plateau. When the compression reaches a certain limit, the force begins to asymptote as we see the strength of the neodymium magnets.
By altering various parameters including:
- Magnet thickness/diameter
- Belleville washer height, inner diameter, outer diameter, tapering, and curvature factors
We are able to optimize the force displacement curve to provide the optimal plateau level and force-ramping.
In conducting many tests and varying the use of different magnet-belleville washer combinations, the following important observations were noted:
- Ridges in force-displacement curve are due to frictional forces encountered during compression of piston.
- In order to optimize plateau characteristics, an even number of belleville washers is required.
- Plateau load cannot be adjusted within single piston; however, ramping slope can be adjusted by increasing initial compressive strain.
Following this proof of concept and the conclusion of my time at the University of Michigan, I partnered with a local medical device company in Ann Arbor to allow them to acquire the technology and move it forward at their discretion.
Reflection
This experience became the cornerstone of my education at the University of Michigan. It helped me connect the worlds of entrepreneurship, engineering, and medicine as I had never known was possible, and for which I was designated as one of 10 Students of the Year at the University of Michigan for the graduating class of 2011. Most of all, the experience showed me how interconnected these fields must be in order for medical breakthroughs to actually benefit society.
As a pre-medical student, I always dreamed of changing the medical field. This experience allowed me to try make impacts in medicine earlier than I had anticipated. It allowed me to work with physicians, and provided a perspective into medicine that many do not see; a side where concepts such as finance and business are equally as important as the medical science for the care of patients.
And while these projects did not “make it big”, they taught me many valuable lessons as an undergraduate that I could not have learned from just the classroom. These skills of independence, creativity, and perseverance would eventually come to help me in my Master’s degree and during my PhD. I credit much of my later success to these early years where I was able to explore and work on my own ideas outside of the classroom.